Nine months after the start of the pandemic, Gov. Laura Kelly issued an executive order requiring testing protocols in Kansas nursing homes, where almost half of the state’s deaths attributed to COVID have occurred. The Dec. 9 order marked her 69th COVID-related order since mid-March but only the second dealing with nursing homes.
“By implementing uniform testing guidelines for nursing facilities statewide, we create clarity on the testing practices that will protect adult care home workers, residents, and communities from the spread of COVID-19,” Kelly said in a press conference earlier this week.
The guidelines require regular testing for long-term care facility staff based on county positivity rates. Nursing homes in counties with a positivity rate less than 5%–the green zone–must test staff once per month. Long-term care staff in counties with positivity rates between 5 and 10%–or the yellow zone–will be tested once per week, and staff in counties with positivity rates higher than 10%–the red zone–will be tested twice per week. Currently, almost all Kansas counties are in the red zone.
Centers for Medicare and Medicaid Services regulates 319 classical, or skilled nursing homes, in Kansas. CMS issued similar testing guidelines for those homes back in August. Under Kelly’s new order, state-licensed facilities will now follow the same rules.
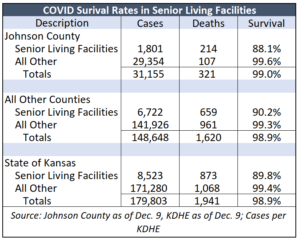 KDHE reports 478 clusters in Kansas nursing homes as of December 9 since the start of the pandemic. The long-term care facilities account for 8,523 COVID cases in Kansas, 723 hospitalizations, and 873 deaths. About 45% of all deaths attributed to COVID deaths to date occurred in long-term care facilities, where the survival rate is 89.9%, versus 99.4% outside of LTCFs.
KDHE reports 478 clusters in Kansas nursing homes as of December 9 since the start of the pandemic. The long-term care facilities account for 8,523 COVID cases in Kansas, 723 hospitalizations, and 873 deaths. About 45% of all deaths attributed to COVID deaths to date occurred in long-term care facilities, where the survival rate is 89.9%, versus 99.4% outside of LTCFs.
Most counties don’t publish this data but the survival rate in Johnson County senior living facilities (a different name but the same definition according to the Johnson County Health Department) is 88.1%, compared to 90.2% in the rest of the state.
The recent executive order marks only the second EO related solely to nursing homes. The first, in April, loosened some licensing requirements for long-term care facilities.
Sen. Richard Hilderbrand, a Galena Republican, wonders if the new order signifies that the Kansas Department of Health and Environment will start providing necessary personal protective equipment (PPE), sanitizing supplies, and testing kits to long-term care facilities.
@sherman_news, Does this mean that @GovLauraKelly, and @KDADSOfficial will finally start following Section 19 of HB 2016, and start providing the necessary personal protective equipment, sanitizing supplies, and testing kits to these facilities? #ksleg https://t.co/4xLNhvTxzR pic.twitter.com/LewBRr4kZn
— Richard Hilderbrand (@Hilderbrand4KS) December 9, 2020
“To this day, I’m still hearing reports that nursing homes are having trouble getting PPE (personal protection equipment). When they order it from the KDHE portal, they’re not getting the quality they need,” he told state officials during a recent Special Committee on Economic Recovery hearing.
The lack of PPE was brought up in September by the Joint Emergency Management Interim Committee.
Little transparency on CARES Act spending
Officials from the Kansas Office of Recovery briefed lawmakers on the committee about their efforts to spend $1.25 billion of federal COVID relief funding. Officials dispersed the money in three rounds, starting with more than $400 million in aid to Kansas counties. They distributed the aid based on population with each Kansas county receiving approximately $194 per resident. Later funding was directed from the state level to public and private entities. In a subsequent round, officials allocated $314 million for statewide investments in education, connectivity, economic development and public health goals. In September, they allocated another $215 million for essential needs, business resiliency and workforce support. The final allocations included $18.5 million for protective and sanitation equipment for nursing homes.
Hilderbrand said Kansas legislators last June adopted statutory language requiring KDHE to provide PPE and other equipment to nursing homes.
“If our main goal is to follow the science and follow the data and we have $1.25 billion for COVID-19, why did we not use that for our most vulnerable?” He asked.
Julie Lorenz, executive director of the Office of Recovery, said the state allocated a total of $45 million for personal protective equipment and supplies. However, there isn’t a clear indication that the PPE is reaching nursing homes.
Back in September, Sen. Dennis Pyle, a Hiawatha Republican, requested a detailed list from the Kelly administration of PPE purchased by the Adjutant General’s office and requests to the Adjutant General’s office from various entities. He asked for the information because he heard nursing homes were unable to obtain PPE but Governor Kelly ordered them to ignore the request.